Members of our Team include:
Glaucoma Fellowship Faculty
Members of our Team include:
Glaucoma Fellowship Research Faculty
Glaucoma Fellowship
The Tradition
More than 180 individuals have obtained clinical and/or research training in glaucoma at the University of California, San Diego. Many of these individuals hold distinguished academic positions and are glaucoma leaders throughout the world. Other fellows have distinguished themselves in their community in clinical practice or in industry.
glaucoma Fellowship
Clinical Experience
Clinical experience consists of participation in glaucoma faculty clinics as well as independent fellows’ clinics at the Shiley Eye Institute in La Jolla and at the UCSD Medical Center in Hillcrest. Fellows gain surgical experience by performing independent and supervised surgery and working with faculty preceptors.
glaucoma Fellowship
Education & Scholarly Activity
The fellow holds an appointment in the UCSD Department of Ophthalmology as Clinical Instructor. Fellows also are expected to actively participate in numerous didactic activities of the Glaucoma Division and the Department of Ophthalmology. The Glaucoma division has monthly journal clubs, lectures, and weekly resident/fellow teaching conferences. There also are weekly Departmental Grand Rounds presentations throughout the year. The fellow will work closely with residents assigned to the Glaucoma service.
In addition to clinical and surgical experiences, all fellows participate in clinical or translational research and will have the opportunity to present their findings at local, regional, and national meetings. Fellows also have the opportunity for involvement in ongoing innovative clinical trials.
Opening in 2003, the Hamilton Glaucoma Center is dedicated to clinical and translational glaucoma research. This 13,500 sq. ft. facility is adjacent to the Shiley Eye Institute. Each fellow has an office on the first floor. The first floor also has space dedicated to clinical research in glaucoma. There, the Imaging Unit at the Hamilton Glaucoma Center is one of the most technologically sophisticated and well-equipped in the world. The second floor has laboratories and additional office space. Our renowned translational science laboratories and faculty investigators are accessible to meet and discuss unmet needs inspired by glaucoma clinical care at UCSD that can lead to project planning and research.
Meet The Glaucoma Faculty
Let's Get Acquainted

ROBERT WEINREB, MD
Robert N. Weinreb, MD. is the Chairman and Distinguished Professor of Ophthalmology at the University of California, San Diego as well as Director of the Shiley Eye Institute and the Director of the Hamilton Glaucoma Center. He also holds the Morris Gleich MD Chair of Glaucoma and is appointed as Distinguished Professor of Bioengineering. Dr. Weinreb graduated from Harvard Medical School and completed his residency and fellowship at the University of California, San Francisco.
Dr. Weinreb is a clinician, a surgeon and a scientist. He oversees all clinical activities at the Shiley Eye Institute and within the Department of Ophthalmology. As the Director of the Hamilton Glaucoma Center, Dr. Weinreb also oversees a world-renowned team of scientists and staff dedicated to glaucoma. Patients from throughout the world seek his medical and surgical expertise.
Dr. Weinreb’s clinical and research interests are diverse and range from the front of the eye to the back of the eye. They include glaucoma surgery, optic neuropathy and aging of the eye, imaging of the optic disc and retinal nerve fiber layer, mechanisms of optic nerve damage in glaucoma, neuroprotection of glaucoma, and cataract surgery.
Dr. Weinreb has delivered more than 140 named lectures and serves on numerous Editorial Boards, including Journal of Glaucoma (Co-Editor), International Glaucoma Review (Chief Editor) and Investigative Ophthalmology and Visual Science. He has trained more than 150 post-doctoral Fellows in Glaucoma, including 21 department Chairs and many others who hold distinguished academic positions in the United States and throughout the world.
His H-impact factor in July 2022 was 138, the highest in world Glaucoma. He also has been cited for several consecutive years by Expertscape as the #1 expert in world glaucoma. Dr. Weinreb has been cited in every edition of Woodward/White, The Best Doctors in America and is an elected member of the prestigious American Ophthalmological Society.

Christopher Girkin, MD, MSPH
Dr. Girkin is an accomplished clinician, scientist, and surgeon who is fellowship trained in both neuro-ophthalmology, with Dr. Neil Miller at Johns Hopkins, and in glaucoma, with Dr. Robert Weinreb at the Hamilton Glaucoma Center.
Following his fellowship training, Dr. Girkin founded the Glaucoma Service and fellowship program at the University of Alabama at Birmingham (UAB). He later served as UAB’s department chair from 2012 to 2022. During his tenure, the department grew to rank in the top five in NIH funding, while integrating with the Callahan Eye Hospital to form UAB Callahan Eye, which was the largest multispecialty ophthalmology group in Alabama.
Dr. Girkin retired from UAB in 2024 and continues his clinical and research work at UCSD, holding the Viterbi Family Endowed Chair for Optic Nerve Biology. Dr Girkin continues an active clinical and surgical practice at the Shiley Eye Institute focusing on complex glaucoma and cataracts.
His research investigates the mechanisms that underlie variations in individual susceptibility to glaucomatous optic neuropathy using patient-based research, health services research, and human tissue studies. Most recently, Dr. Girkin’s lab has developed a novel ocular hypertension model in the post-mortem human eye, which he is using to define the cellular responses to IOP change in the human eye for the first time.
Dr. Girkin’s work has resulted in extensive publications, and he has received continuous NIH funding for over 20 years. He has lectured extensively to practitioners and researchers worldwide, including providing the 2025 American Glaucoma Society Clinician-Scientist Lecture. He has served in multiple national leadership roles, including serving as President of the American Glaucoma Society.

ALEX A. HUANG, MD, PHD
What I took away from my glaucoma fellowship
Glaucoma fellowship is the most critical of “next steps” in our careers. In residency, we make life-long relationships, but we also all move in different directions in terms of clinical interest, scholarly pursuits, and personal life. Glaucoma fellowship builds a different kind of family. We are forever linked, not simply based on past shared experiences, but moving in the future: the next challenging glaucoma clinical case, glaucoma research question, or professional advancement hurdle.
Personally, I am a former glaucoma fellow at UCSD, and I am forever grateful to have joined a huge family of glaucoma clinicians, researchers, and leaders throughout the world. This family has not only supported me in my education and career growth, but I also know that I am only one family call away from a true world’s expert for any glaucoma question in the future.
Biography
Dr. Alex Huang is the newest member of the glaucoma division at the Viterbi Family Department of Ophthalmology and Shiley Eye Institute. He completed his MD / PHD at The Johns Hopkins School of Medicine, his ophthalmology residence at the then Doheny Eye Institute and University of Southern California.
Dr. Huang is a former UCSD glaucoma fellow. After fellowship, he became one of the founding members of the Doheny Eye Institute and UCLA affiliation where he also served as the Director of Ophthalmology at the City of Hope Cancer Center. Today, Dr. Huang is a clinician-scientist supported by the NIH and NASA where he studies fluid flow in around the eye for intraocular pressure regulation as well as optic disc edema of astronauts on the International Space Station.

SASAN MOGHIMI, MD
Dr. Moghimi completed a residency in ophthalmology at Farabi Eye Hospital, and subsequently served as Professor and Vice-Chair. He completed fellowships in glaucoma at UC Los Angeles, and UC San Francisco. Dr. Moghimi has an active clinical practice managing adult glaucoma patients and complex cataract surgeries. Dr. Moghimi’s clinical focus is glaucoma including angle closure glaucoma. He is also running myopia and glaucoma clinic with complex diagnostic and management cases.
Dr. Moghimi’s research focuses on functional and structural measurements for optimizing diagnosis of glaucoma or its progression with a focus in advance glaucoma, use of artificial intelligence approaches in glaucoma diagnostics, and study of angle closure disease. He has been the recipient of many awards including the UC Tobacco-Related Disease Research Program, and NIH R01 awards.
Dr. Moghimi is a clinician-scientist who continues to teach and publish extensively. He has several educational awards including outstanding Clinical Teaching Award. He has co-authored over 200 peer-reviewed journal articles and book chapters related to glaucoma and vision science. He is an editorial board member of many ophthalmology journals including Investigative Ophthalmology & Visual Science and, International Glaucoma Review.
My philosophy has been developed through 15 years of teaching residents and glaucoma fellows, and through my role as vice-chair for education early in my career. It’s very simple, as a clinical teacher you learn more from fellows and residents when you teach. I believe careful observation, reading, and creative thinking during practice are the keys to fast learning of the producers. I am rewarded by seeing our fellows bloom into the best glaucoma surgeons in the nation.

CRISTIANA VASILE, MD
What I Took Away From My Glaucoma Fellowship
My glaucoma fellowship was transformative. It challenged me to grow as a clinician and deepen my empathy for patients navigating life with chronic vision loss. Surgically the fellowship was a masterclass in precision and adaptability. From traditional procedures like trabeculectomy to MIGS, I gained hands-on experience that taught me not only technique, but judgement – how to intervene, how to manage complications, and how to counsel patients through uncertainty.
Equally important, was the growth in my professional independence. I learned to trust my instincts and to embrace flexibility and resourcefulness. Through the mentorship I received and the collaboration I formed, I gained a broader perspective on innovation and a professional network to excel. In sum, my glaucoma fellowship was not just a training ground – it shaped me into a more mature, thoughtful, skilled and compassionate physician. This fellowship didn’t just refine my skills – it clarified my purpose. The lessons I carry forward are not only technical but deeply human.
Biography
Cristiana Vasile, MD, MAS is a Board-Certified Ophthalmologist and Fellowship trained Cataract and Glaucoma specialist. Dr. Vasile is a graduate of Bucharest University of Medicine. She spent several years at the Hamilton Glaucoma Center, UC San Diego Shiley Eye Institute doing vision research and served as the founding Director of the UC San Diego Optic Nerve Reading Center. Prior to her internship and residency, she completed a Masters in Advanced Studies (MAS) in Clinical Research at UC San Diego.
Subsequently, she completed the Residency in Ophthalmology at UC San Diego and she was the recipient of the UC San Diego Resident Research Award. She then completed a Glaucoma Fellowship at UC San Diego. After fellowship, her research continues to focus on structure and function of the optic nerve. Her work has been published in peer-reviewed ophthalmology journals and she has authored several book chapters.
Meet the Glaucoma Research Faculty
Introductions

Sally Baxter, MD, MSc
Sally L. Baxter, MD, MSc is a comprehensive ophthalmologist whose research includes a strong emphasis on glaucoma. She is the Chief of the Division of Ophthalmology Informatics and Data Science at the University of California San Diego Viterbi Family Department of Ophthalmology and Shiley Eye Institute.
She is a recipient of the 2020 NIH Office of the Director Early Independence Award and was named in the “40 under 40” list by Ophthalmology Management as well as the "Power List - Rising Stars" in The Ophthalmologist. She received the 2023 NEI Director's Award and the 2024 ARVO Foundation Ludwig von Sallmann Clinician-Scientist Award.
She is a member of the American Academy of Ophthalmology Committee on Artificial Intelligence and chairs the AAO workgroup on data standards.Her research is focused on big-data analytics, artificial intelligence, and applied informatics for optimizing clinical workflows.
She also leads several training programs aimed at expanding the future workforce for both ophthalmology and informatics/data science.
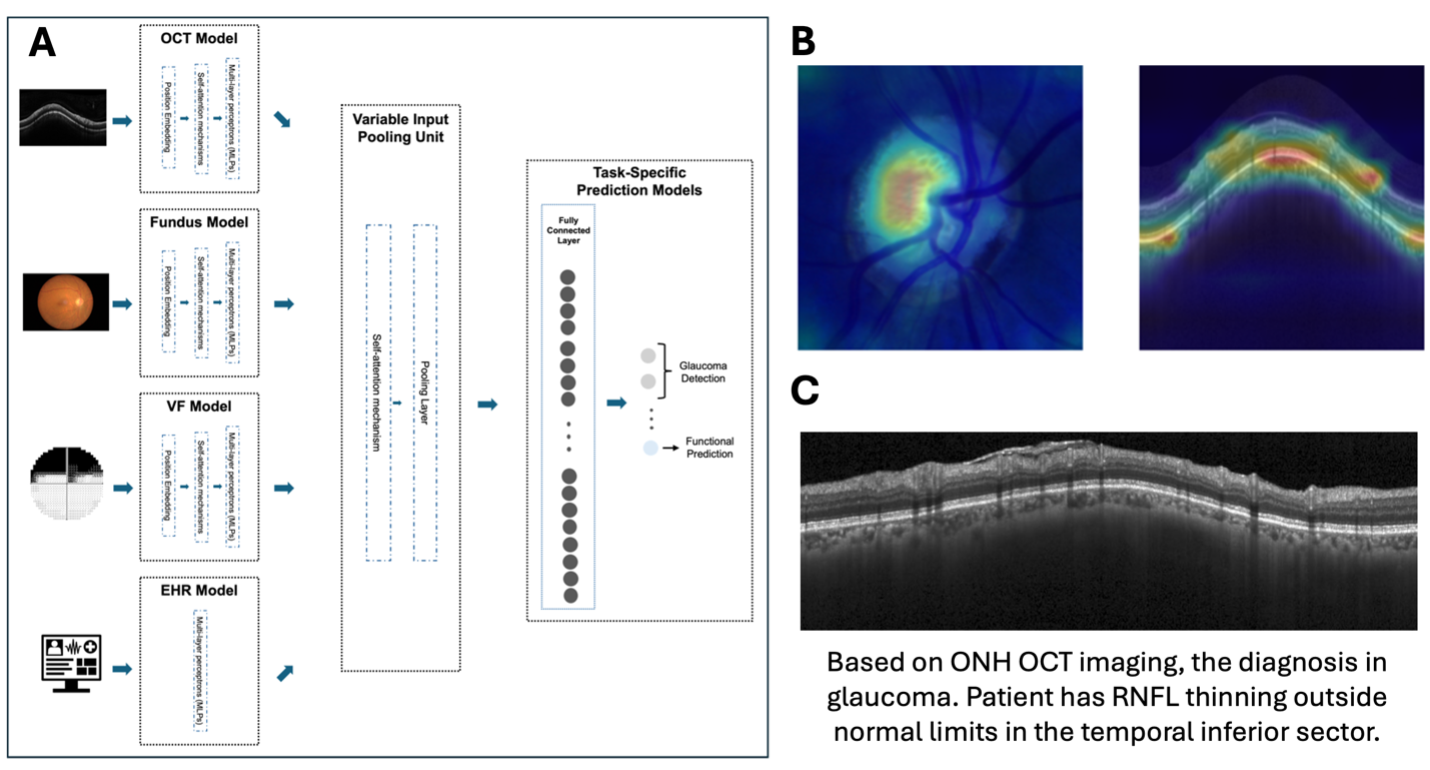
Figure 1: We apply multimodal predictive and g AI methods (A) to detect disease, predict progression, identify impactful structural features (B), and provide clinical decision support (C), among many other tasks.
Mark Christopher, PhD
Dr. Mark Christopher focuses on applying AI methods to clinical ophthalmic care, especially in glaucoma. Dr. Christopher’s lab uses a variety of AI and computational techniques along with longitudinal, multi-modal datasets to address unmet needs in ophthalmology. This includes developing models for diagnosis and screening, predicting visual function, identifying disease progression, and forecasting the need for medical / surgical interventions, as well as other clinically relevant tasks.
Dr. Christohper’s team also applies generative AI models to help review medical images and provide clinical decision support. Their current work is focused on evaluation and deployment of these approaches in real-world clinical settings.

Figure: Optic nerve transplanted NSCs extend axons into the optic chiasm.
Jiun Do, MD, PhD
Research in the Do lab focuses on the development of treatments to regenerate the optic nerve and facilitate the success of vision restorative whole eye transplantations. Using novel applications of stem cell techniques and technologies, we are pioneering the development of optic nerve neuronal relays to restore connections between the eye and the brain. In in vivo experiments, we have demonstrated the generation of long-distance, stem cell-derived axons that project from an optic nerve injury site beyond the optic chiasm and into vision associated targets in the brain.
Ongoing work seeks to demonstrate the recovery of functional vision following the treatment of transected optic nerves with stem cell-derived optic nerve relays. Future efforts will use combinatorial approaches including CRISPR-based gene editing and gene therapies to complement the vision restorative effects of optic nerve neuronal relays.
Ultimately, this work will enable whole eye transplants and the ability to restore vision to people with severe visual impairments or blindness.
Biography
Dr. Jiun Do is an Assistant Adjunct Professor of Ophthalmology at the Viterbi Family Department of Ophthalmology and Shiley Eye Institute. He earned his MD and PhD in Neurosciences from the University of California San Diego. Dr. Do completed his ophthalmology residency at the University of Southern California Roski Eye Institute and his glaucoma fellowship at the University of California San Diego Shiley Eye Institute and the Hamilton Glaucoma Center.
Following fellowship, he joined the faculty at the Shiley Eye Institute as a clinician-scientist. Dr. Do is supported by the NIH support to develop stem cell-based methods to regenerate the optic nerve and restore vision. He is also engaged in clinical research and clinical trials in the management of glaucoma.
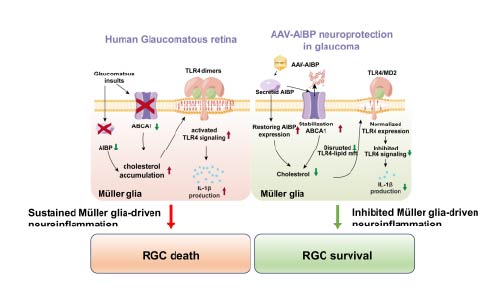
Figure: Protective effect of AIBP on mitochondrial dysfunction and glia-driven neuroinflammation induced by glaucomatous insults. PMID: 40349106 DOI: 10.1016/j.ymthe.2025.05.009
Wonky Ju, PhD
Dr. Wonkyu “Daniel” Ju, PhD, Professor and Hanna and Mark Gleiberman Chancellor’s Endowed Chair in Glaucoma Research in the Viterbi Family Department of Ophthalmology and the Shiley Eye Institute (SEI), is an internationally recognized leader in gene therapy and mitochondrial biology for glaucoma and neurodegenerative eye diseases.
Dr. Ju’s research focuses on unraveling how mitochondrial dysfunction, neuroinflammation, and neurodegeneration drive glaucomatous optic neuropathy. His lab is pioneering adeno-associated virus (AAV)-based gene therapies beyond conventional glaucoma treatments, primarily aiming to lower intraocular pressure. By targeting the underlying biological causes of disease progression, his work promises to transform how glaucoma is treated.
A key focus of Dr. Ju’s research is developing gene therapies that: 1) reduce retinal neuroinflammation, 2) protect retinal ganglion cells and glial cells from neurodegeneration, and 3) address mitochondrial dysfunction and protection in glaucoma. His team is investigating the crucial role of glia-driven neuroinflammation, neurodegeneration, and neuroprotection in optic nerve damage and retinal ganglion cell death.
By leveraging advanced animal models and precision gene delivery systems (AAV and lentiviral vectors), they aim to protect retinal ganglion cells and glial cells, ensuring both safety and therapeutic efficacy. Through detailed studies of transgene expression and function, Dr. Ju’s research bridges laboratory breakthroughs with real-world clinical applications—bringing us closer to effective, disease-modifying treatments for glaucoma patients worldwide.
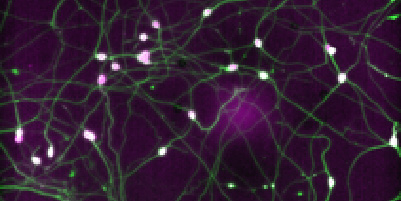
Figure: Protective effect of AIBP on mitochondrial dysfunction and glia-driven neuroinflammation induced by glaucomatous insults. PMID: 40349106 DOI: 10.1016/j.ymthe.2025.05.009
Karl Wahlin , PhD
My overarching interests are understanding how the human retina forms, why retinal neurons degenerate during disease, and ultimately, how to restore vision after the retina has already failed. My interests range from neuroprotection and retinal development to retinal degenerative (RD) diseases such as glaucoma, Leber’s congenital amaurosis, retinitis pigmentosa, and age-related macular degeneration.
My group leverages CRISPR-based gene-editing to create stem cell-based human retinal models with reporters capable of giving real-time information on retinal cell fate. With these tools, we have developed in vitro models of human retinal development using 3D retinal organoids, which we have improved by incorporating small-molecule drugs and optimizing the cellular microenvironment. The result is organoids with greatly improved reproducibility in terms of size and cellular composition.
In addition, my lab has used multi-omics approaches to study RNA, microRNAs, and the chromatin landscape of developing retinas and will use this new information to advance the field of endogenous regeneration of human retinas.
Using these tools, we explore retinal cell fate decisions by engineering PSCs with transgene cassettes capable of delivering cell-type-specific transcription factors; one recent study identified a 4-gene combination that greatly facilitated retinal ganglion cell formation for glaucoma. Finally, we are greatly interested in exploring reparative therapies by exploring endogenous regeneration of Müller cells, which is a central focus of studies aimed at regenerating both retinal ganglion cells and photoreceptors.

Linda Zangwill, PhD
Dr. Linda Zangwill leads a clinical research team dedicated to advancing the understanding of structural and functional changes in the aging and glaucomatous eye.
Her team integrates optical coherence tomography imaging, visual function testing, and rich clinical and demographic data to develop innovative methods for distinguishing highly myopic eyes with and without glaucoma.
They also apply artificial intelligence and machine learning techniques to improve glaucoma detection and identify individuals at highest risk of vision loss.
Dr. Zangwill’s group actively collaborates in several large international consortia focused on glaucoma, myopia, and AI-driven approaches to prevent blindness.
Glaucoma Fellowship
Success After Fellowship
Firsthand accounts of an amazing experience

ANDREA YONGE, MD
There is much to learn during one short year of glaucoma fellowship: clinical management and data interpretation, surgical techniques (traditional glaucoma surgery, minimally invasive glaucoma surgery, and complex cataract surgery), and patient education/communication skills. When I was applying to glaucoma fellowship programs, the Shiley Eye Institute at UCSD was at the top of my list.
Under the tutelage of Dr. Robert Weinreb, a world expert in glaucoma treatment and research, as well as the rest of the glaucoma faculty, I was able to gain a strong foundation in clinical and surgical management of glaucoma. There are few programs in the country that offer training in not only traditional glaucoma surgery (particularly the art of the trabeculectomy) but also minimally invasive glaucoma surgery (angle surgery and subconjunctival filtration surgery) as well as cataract surgery. I am so grateful for the mentorship and training that I received at UCSD, and I look forward to seeing future generations of glaucoma fellows carry on the legacy of excellence.
After fellowship, I will be joining a physician-owned private practice in Portland, Oregon. There is a large population of patients with glaucoma in the area and few fellowship-trained glaucoma specialists. My fellowship training at UCSD has prepared me to provide efficient and high-quality patient-centered care in the areas of cataract, glaucoma, and comprehensive ophthalmology. I have experience with complex cataract surgery, premium intraocular lenses, and nearly all types of glaucoma surgery. I also feel prepared to learn and adopt new techniques as the landscape of glaucoma surgery evolves in the coming years.
After 10 years of medical education, I am excited for the opportunity to establish myself as a cataract and glaucoma specialist within my new community. In my free time, I hope to explore the endless hiking trails in Oregon and spend more time connecting with nature.

Adele Yarmohammadi, MD
It is an absolute honor to be able to train under the mentorship of one of the most prominent leaders in the field, Dr. Weinreb, as well as other esteemed faculty at UC San Diego Shiley Eye Institute. The clinical and surgical experience is simply outstanding. I am beyond grateful to be able to learn such a diverse set of surgical procedures to provide the best possible care to my future patients. If I go back in time, I will again rank UCSD as my number one fellowship choice without question.
Glaucoma Fellowship
Our Locations
Shiley Eye Institute
The Viterbi Family Department of Ophthalmology and Shiley Eye Institute operating rooms are conveniently located on the third floor of the Shiley Eye Institute building. This allows convenient access between clinical outpatient and surgical spaces for constant and seamless patient care between the two. The OR is thoughtfully designed with a spacious waiting area and both pre- and post-op spaces conducive to efficient case turn-over as well as patient satisfaction.
Fellows should anticipate spending 1-2 days a week in the operating rooms. Fellows have a robust surgical experience with a wide variety of surgical procedures including:
· MIGS procedures (iStent, OMNI, Hydrus, trabectome, and XEN)
· Cataract and glaucoma surgery
· Trabeculectomy with and without anti-metabolite
· Glaucoma drainage device
· Laser diode cyclophotocoagulation (standard and micropulse)

Shiley Eye Institute

UCSD Medical Center in Hillcrest and Ophthalmology Clinic

Viterbi Family Department of Ophthalmology and Shiley Eye Institute operating rooms

Hamilton Glaucoma Center with the Clinical Research Space, Glaucoma Surgical Innovations Lab and Training Center, and Fellow Offices

San Diego is known for its year-round ideal climate, averaging about 55ºF in January to 73ºF in August. This means that San Diego is an outdoor and sporting paradise where you can enjoy the sun, surf, mountains, deserts, and international flavor of our city.
Glaucoma Fellowship
Apply Today
Applicants for fellowship training in Glaucoma who have completed an ACGME residency in the US (and Canada, if eligible for California licensure) must register for the Ophthalmology Fellowship Match online (sfmatch.org) by submitting the required application and supplemental materials listed therein.
SF MatchThe deadline for this process is September 15 of the year prior to the start of the desired fellowship-training year. The fellow must be eligible for a California Medical License, as medical licensure from the California Medical Board is required (mbc.ca.gov).
International applicants for glaucoma fellowship are considered outside of the SFMatch and should contact Marlene Virgen at mvirgen@health.ucsd.edu for additional information. These positions focus on glaucoma research with an opportunity for clinical activities.
More Information
